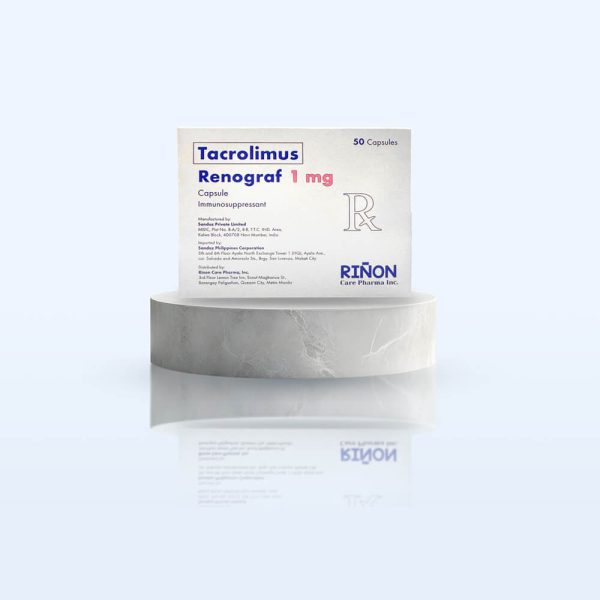
Description
Bioavailability and Pharmacokinetics
Pharmacotherapeutic group: Immunosuppressants, calcineurin inhibitors. ATC code: L04AD02.Pharmacology: Pharmacodynamics: Mechanism of action: At the molecular level, the effects of tacrolimus appear to be mediated by binding to a cytosolic protein (FKBP12) which is responsible for the intracellular accumulation of the compound. The FKBP12-tacrolimus complex specifically and competitively binds to and inhibits calcineurin, leading to a calcium-dependent inhibition of T-cell signal transduction pathways, thereby preventing transcription of a discrete set of cytokine genes.Pharmacodynamic effects: Tacrolimus is a highly potent immunosuppressive agent and has proven activity in both in vitro and in vivo experiments.In particular, tacrolimus inhibits the formation of cytotoxic lymphocytes, which are mainly responsible for graft rejection. Tacrolimus suppresses T-cell activation and T-helper-cell dependent B-cell proliferation, as well as the formation of lymphokines (such as interleukins-2, -3, and γ-interferon) and the expression of the interleukin-2 receptor. Clinical efficacy and safety: Results from clinical trials performed with once-daily tacrolimus: Liver transplantation: The efficacy and safety of tacrolimus prolonged-release and tacrolimus immediate-release, both in combination with corticosteroids, was compared in 471 de novo liver transplant recipients.
The event rate of biopsy confirmed acute rejection within the first 24 weeks after transplantation was 32.6% in the tacrolimus prolonged-release group (N=237) and 29.3% in the tacrolimus immediate-release group (N=234). The treatment difference (prolonged-release - immediate-release) was 3.3% (95% confidence interval [-5.7%, 12.3%]). The 12-month patient survival rates were 89.2% for tacrolimus prolonged-release and 90.8% for tacrolimus immediate-release; in the tacrolimus prolonged-release arm 25 patients died (14 female, 11 male) and in the tacrolimus immediate-release arm 24 patients died (5 female, 19 male). 12-month graft survival was 85.3% for tacrolimus prolonged-release and 85.6% for tacrolimus immediate-release.Kidney transplantation: The efficacy and safety of tacrolimus prolonged-release and tacrolimus immediate-release, both in combination with mycophenolate mofetil (MMF) and corticosteroids, was compared in 667 de novo kidney transplant recipients. The event rate for biopsy-confirmed acute rejection within the first 24 weeks after transplantation was 18.6% in the tacrolimus prolonged-release group (N=331) and 14.9% in the tacrolimus immediate-release group (N=336). The treatment difference (prolonged-release - immediate-release) was 3.8% (95% confidence interval [-2.1%, 9.6%]).
The 12-month patient survival rates were 96.9% for tacrolimus prolonged-release and 97.5% for tacrolimus immediate release; in the tacrolimus prolonged-release arm 10 patients died (3 female, 7 male) and in the tacrolimus immediate-release arm 8 patients died (3 female, 5 male). 12-month graft survival was 91.5% for tacrolimus prolonged-release and 92.8% for tacrolimus immediate-release.Distribution: In man, the disposition of tacrolimus after intravenous infusion may be described as biphasic. In the systemic circulation, tacrolimus binds strongly to erythrocytes resulting in an approximate 20:1 distribution ratio of whole blood/plasma concentrations. In plasma, tacrolimus is highly bound (> 98.8%) to plasma proteins, mainly to serum albumin and α-1-acid glycoprotein. Tacrolimus is extensively distributed in the body. The steady-state volume of distribution based on plasma concentrations is approximately 1300 L (healthy subjects). Corresponding data based on whole blood averaged 47.6 L. Biotransformation: Tacrolimus is widely metabolized in the liver, primarily by the cytochrome P450-3A4. Tacrolimus is also considerably metabolized in the intestinal wall.
Dose range
Known adverse effects and toxicities
Special precautions
Graft rejection or other side effects which could be a consequence of either under- or overexposure to tacrolimus. Prophylaxis of transplant rejection in adult heart allograft recipients. Suspected symptoms or signs of GI perforation. Cardiomyopathies may occur. May prolong the QT interval & cause Torsades de Pointes. Patients w/ risk factors for QT prolongation including those w/ personal or family history of QT prolongation, CHF, bradyarrhythmias & electrolyte abnormalities; diagnosed or suspected to have congenital long QT syndrome or acquired QT prolongation, or on concomitant medications known to prolong the QT interval, induce electrolyte abnormalities or known to increase exposure. Development of EBV-associated lymphoproliferation disorders or posterior reversible encephalopathy syndrome. Limit exposure to sunlight & UV light due to risk of malignant skin changes. Eye disorders (sometimes progressive to loss of vision). Increased risk for infections including opportunistic infections eg, BK virus associated nephropathy & JC virus associated progressive multifocal leukoencephalopathy; viral hepatitis. Pure red cell aplasia.





Reviews
Clear filtersThere are no reviews yet.